Did you know that you can take an active role in managing your care? Consider beginning with utilizing the best technologies available. Insist on a non-contrast, low cost, MRI with AI-assisted interpretation by ProstatID™ PRIOR to agreeing to any biopsy because ProstatID™ better detects true cancers and reduces false positives, saving you time, expense, and avoidance of unnecessary procedures.
Prostate Care is rapidly evolving and improving. The use of MRI is quickly changing the standard of care with an increasing number of urologists seeking MRI before they decide to biopsy in lieu of taking a standard 12-core biopsy first. And, more importantly, you may not need a biopsy, and you certainly want to avoid it if not needed as the experience and side effects are not pleasant. With the help of AI such as ProstatID, MRI is proving to significantly reduce the number of unnecessary biopsies performed on false indications. Additionally, ProstatID has proven in clinical studies to not only reduce the number of false positives but also increase the number of early cancer detections. On the other hand, if a detection is presented, then the AI output provides the interventionalist with an excellent means of targeting the suspect tumor.

Benefit from using Artificial Intelligence
You can benefit from using Artificial Intelligence significantly aiding prostate cancer detection and diagnosis.
Learn about ProstatID does just that.
Empowering both patient and physician alike.
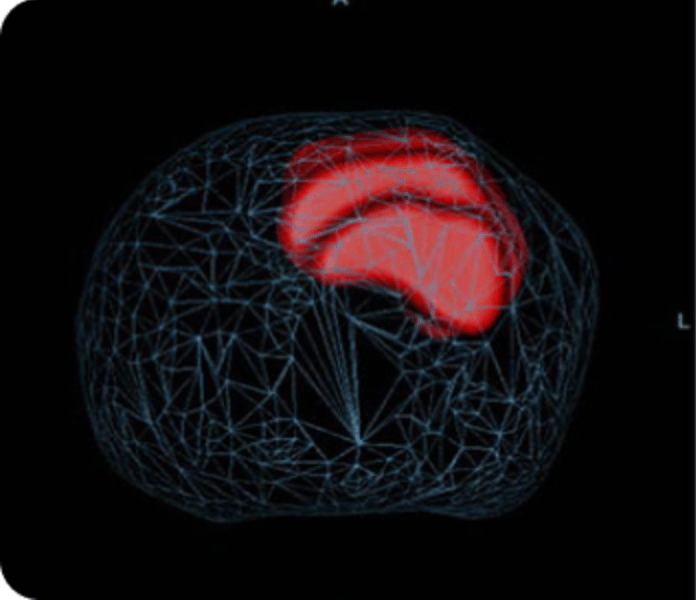
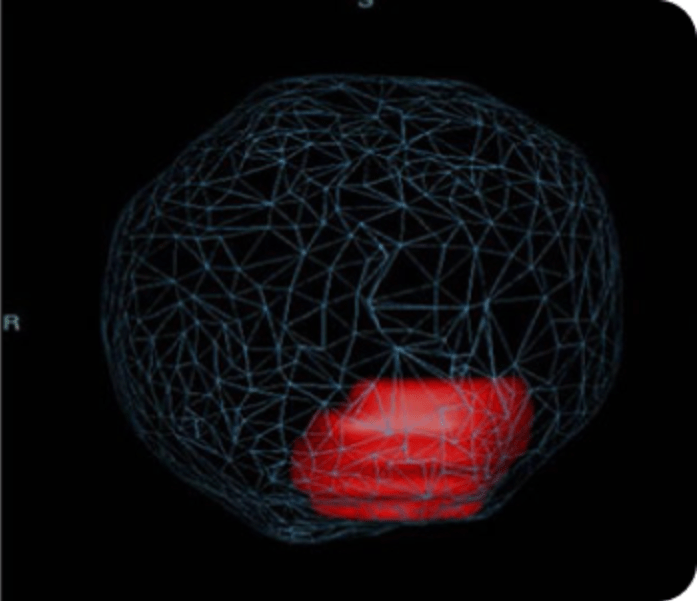
Provide patients with more information, easily visualized in 2D and 3D thus increasing personal involvement in care choices.
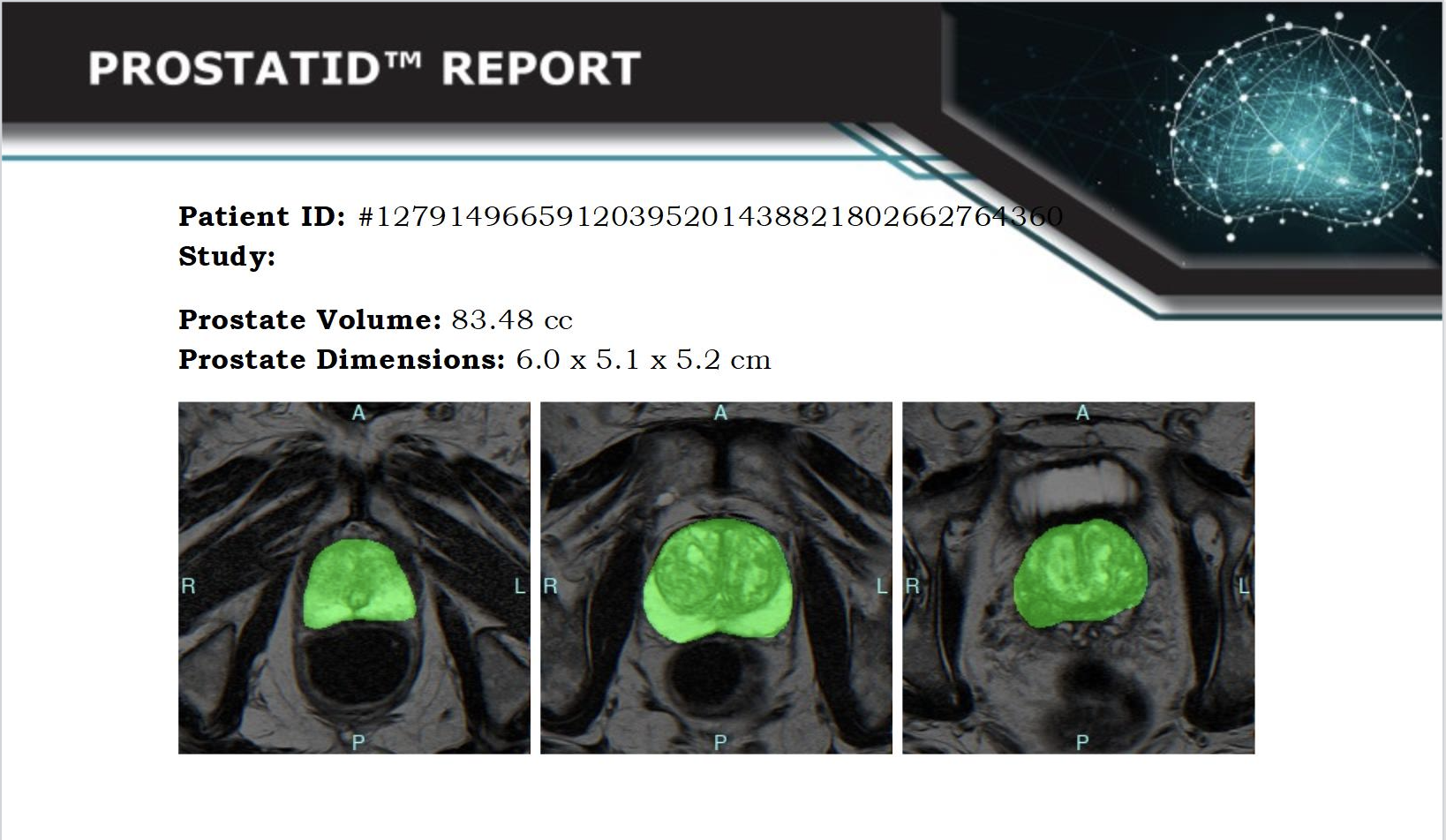
There is nothing more welcome by a patient than receiving a clean bill of health such as the patient did with this ProstatID report – Green is Good = Normal!
This patient presented with many of the symptoms of prostate cancer: frequent urination, incomplete voiding and lower back pain but these symptoms were not cancer but caused by an enlarged prostate with significant BPH (benign prostate hyperplasia), of which there are numerous non-threatening treatments.
How ProstatID Works
Scan
Technologist performs standard screening or diagnostic MRI sequences and pushes the study to their PACs with is Standard Operating Procedure. In parallel, they push the study to the Platform partner of cloud service provider.

Detect
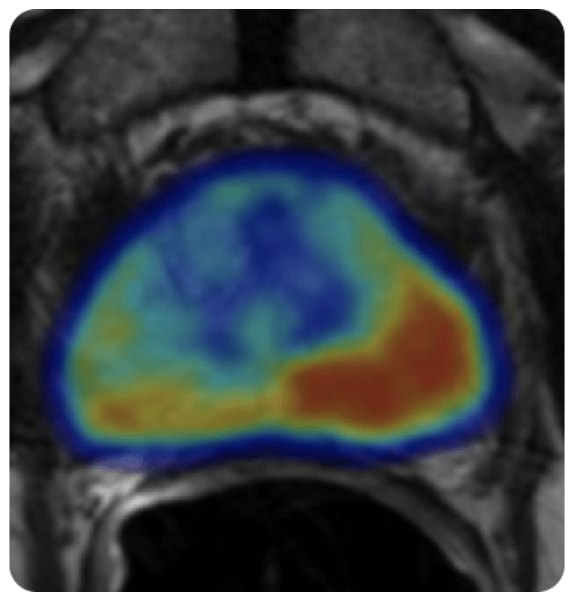
ProstatID automatically detects study, sorts for necessary sequences, checks quality, performs the detection and diagnosis and returns an appended series to the unique patient ID with results and report to view in less than 5 minutes typically = real-time diagnosis.

Diagnose
This new series and report are appended to the study so that the radiologist sees it along with all others on his/her viewing station; hence, no additional effort, equipment or work to perform.

Treat or
Don’t Treat
ProstatID assists physicians with treatment planning by providing an entire view of the organ highlighting all suspicious lesions with their individual risk scores. Additionally, if lesion(s) are graded as high risk, they are presented in two powerful 3D views within a transparent rendition of the prostate gland giving interventionalists ideal cognitive targeting.

With changes in technology occurring rapidly and often, it is challenging for physicians to keep up. Therefore, ask your PCP, radiologist or urologist about using the ProstatID AI for your MRI study and ask them to refer to this website for more information if they have not heard of it and for more information.
Talk to your doctor about Bot Image™'s ProstatID and how it can significantly improve your diagnosis and treatment planning.
You can and should insist on receiving the best quality of care so you are encourage to seek other options to cancer diagnosis with MRI and AI as well as more informed treatment planning and state-of-the-art tools and expert physicians. Learn about our Prostate Centers of Excellence and Concierge Medicine Coalition HERE: