Our Story
Bot Image™, Inc. is a medical imaging software company that utilizes artificial intelligence technology for magnetic resonance imaging interpretation.
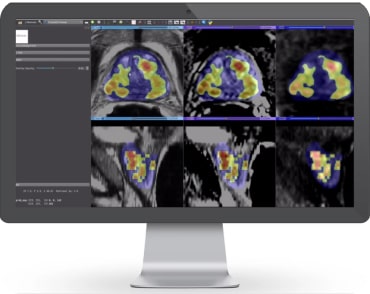
ProstatID™ is a radiological computer assisted detection (CADe) and diagnostic (CADx) software-only device for use in a healthcare facility or hospital to assist trained radiologists in the detection, assessment and characterization of lesions suspicious for cancer using MR image data. The software automatically registers images, then segments and analyzes the central gland and entire prostate organ. It identifies suspicious abnormalities by employing a pixel-wise random forest learning-based method based upon various features referenced to ground truth data on which it was trained.
Modeled after popular Breast Cancer AI, ProstatID is the first and only software FDA-cleared for not only prostate cancer detection and diagnosis but screening using non-contrast MRI.
Our Technology
Bot Image™’s software interprets multi-parametric and bi-parametric MRI using random forest with instance weight and MR segmentation by deep learning with holistically-nested networks. ProstatID™ was trained from thousands of proprietary MR image sets, radiologist interpretations, segmented prostate gland image sets, pathology laboratory results, correlation data, and first-pass AI interpretations to aid in the early diagnosis of prostate cancer.
Outputs of the software include a colorized overlay of a copy of one of the input image series highlighting the boundaries of suspicious lesions and grading them according to the software’s proprietary probability index value and PI-RADS score. These outputs provide whole gland assessment for treatment planning and interventional guidance.
Our Vision
Bot Image™, Inc. brings early detection of prostate cancer using MRI and AI to the forefront of medicine. Our highly advanced, non-invasive technology shows promise of delivering high 90th percentile sensitivity in detection, as well as, specificity (accuracy) with the near elimination of false positives and false negatives. Once refined, we will then utilize the same baseline AI algorithms to address the early diagnosis of other cancers and COPD.
About The Team

Dr. Randall W. Jones (PhD, MBA)
CEO & FOUNDER

Dr. Randall W. Jones, D.E. (PhD, MBA) | Founder, CEO and Board Chair
Dr. Jones, a USAF Cold war veteran evolved into a prolific medical device inventor and serial entrepreneur, has translated his experiences & academic training into advanced, innovative medical device development. Previously, as Founder and CEO of ScanMed LLC, Dr Jones launched a technology startup in his garage that ultimately attained the status of the world’s largest independent MRI antenna (coil) design, manufacturing and maintenance company.
Subsequently, Dr. Jones applied his growing skill sets to launch Bot Image™ and rapidly grew the company into an industry-leader in the field of Artificial Intelligence (AI) based software development. Within two years of its launch, Bot Image obtained a unique trifecta of FDA clearance for the detection, diagnosis and screening of prostate cancer. Dr. Jones is animated by a passion to drive the positive transformation of healthcare through the intelligent application of breakthrough technologies that greatly enhance early disease detection, treatment planning & patient care.

Paul Pfeiffer
Chief Commercial Officer

Paul Pfeiffer | Chief Commercial Officer
Paul Pfeiffer serves as Chief Commercial Officer at Bot Image™, where he is responsible for the company’s Commercialization strategy and Sales functions. As a 30-year veteran in the Diagnostic Imaging Industry, Paul has been a top performer for some of the industry’s leading companies. Upon completing a tour of duty in U.S. Army, Paul started his career in MRI coil technology with roles in manufacturing, design, and engineering leadership with both Medical Advances and GE. That core understanding of the technology made the transition into sales and marketing a natural one. Paul held various roles at Toshiba/Canon culminating as the National Sales Director for their CT product line. Most recently Paul was the Keystone Regional Vice President of Sales for Siemens Healthcare when he and his team delivered unprecedented growth in market share and sales volume over his tenure. Keeping the focus on customer satisfaction and delivering growth beyond expectations has been the keys to his success.

Mike Buck, CPA
CHIEF FINANCIAL OFFICER

Mike Buck | CPA, MBA, & CFO
Specializes in Start-up and MedTech Finances. With extensive experience as a Professor of Accounting & Finance and a solid foundation as a Senior Accountant at KPMG, Mike brings invaluable knowledge to the table. With 25+ years of experience in managing his own Accounting firms, he excels in business consulting, tax compliance, and has guided various startups from inception to acquisition. Moreover, Mike is deeply engaged in the entrepreneurial community, actively mentoring many entrepreneurs and fostering innovation and growth within the startup ecosystem and economy.

Melanie Jones
Board Member and EVP Sales & Marketing

Melanie Jones | Board Member and EVP Sales & Marketing
Melanie has spent her entire career within the sales arena. Beginning with a number of years as an Account Executive selling to National Accounts with Sprint then moving into the emerging call center space. Her experience including working with very large call center providers selling inbound and outbound services as well as selling for mid-size and small start up organizations. Key clients included Bank of America, Worldcom Wireless, Ameritech to name a few. Melanie transferred her skill set to ScanMed LLC selling within the MRI industry to hospitals, OEMs and imaging centers across the globe resulting in obtaining contracts with MRI world leaders such as Siemens Healthcare. She then brought those medical arena experiences and insights to Bot Image™ in her role as EVP Sales and Marketing while also serving on the Board of Directors.

Donna Gurley
Communications Director and Quality Manager

Donna Gurley | Communications Director and Quality Manager
Donna has worked in accounting and administration in a number of industries for 30+ years, most notably in medical hardware for 6 years. Joining Bot Image at its inception, Donna provides support for the functional areas of the company and manages the Quality and Regulatory Compliance aspects of the business.

Dr. Eric Walser, M.D.
Radiologic Interventionalist Advisor

Dr. Eric Walser, M.D. | Radiologic Interventionalist Advisor
Dr. Walser is the John Sealy Distinguished Chairman and Professor of Radiology at University of Texas Medical Branch, Galveston, Texas. An Interventional and Diagnostic radiologist, Dr. Walser brings his world-leading expertise in prostate cancer diagnosis & treatment to Bot Image™. Dr. Walser was a pioneering early adopter of focal radio frequency ablation of prostate cancer, a technology with demonstrated performance in the elimination of cancer while leaving the prostate intact with full functionality. In spite of these proven benefits, focal radio frequency ablation is not yet approved for insurance reimbursement. However, through ongoing research and innovation in practice, Dr. Walser continues to contribute to the science & education of prostate cancer detection and treatment. Activities such as Dr. Walser’s are impactful in positively changing the healthcare paradigm.

Dr. D. Russell Locke, M.D.
Urologic Advisor

Dr. D. Russell Locke, M.D. | Urologic Advisor
D. Russell Locke, M.D., FACS, is a luminary in the field of urology, serving as the Founder and Director of the Vantage Urologic Institute in Ocala, Florida. His expertise is notably distinguished in the arenas of urologic oncology, emerging minimally invasive therapies for prostate disease, and the enhancement of male sexual health.
Board-certified by the American Board of Urology and a Fellow of the American College of Surgeons, Dr. Locke is a vibrant contributor to regional and national medical communities. Dr. Locke’s commitment to clinical research and patient care is particularly evident in his approach to the nuanced areas of prostate cancer diagnosis and risk stratification. He is an advocate for structured active surveillance for patients with low-risk prostate cancer and champions noninvasive focal ablation therapies for localized tumors.
Since establishing his practice in 1988, Dr. Locke has consistently introduced innovative technologies and surgical methods that have shaped the regional landscape of urologic healthcare.
In his advisory role at Bot Image™, Inc., Dr. Locke’s extensive experience and forward- thinking mindset are invaluable assets in the company’s mission to revolutionize the early detection of prostate cancer using AI-enhanced MRI technology. His guidance is pivotal in harnessing the potential of ProstatID™ to set new standards in diagnostic accuracy, offering hope for early and precise intervention in prostate cancer and beyond.

Jerry Kolosky
Corporate Strategist and Board Member

Jerry Kolosky | Corporate Strategist and Board Member
As digital health visionary and innovator, Mr Kolosky has dedicated his career to the development of an intelligent, technology-enabled healthcare ecosystem designed to meet the challenges of global population health & chronic disease management with a focus on improved outcomes, cost efficiency, enhanced patient engagement and optimized clinical resource utilization across the continuum of care.
Throughout his career, Mr Kolosky has held executive and consulting positions with global technology companies, digital health startups, tech incubators & prominent foundations. Mr Kolosky is also active in the US healthcare policy arena, offering subject matter expertise & counsel to US Congressional & Senate Sub-Committees, CMS, and a variety of digital health advocacy coalitions.

Tim Manion
Financial Advisor and Board Member

Tim Manion | Financial Advisor and Board Member
Mr. Manion has over 39 years’ experience in both international and domestic financial management in the investment banking, real estate, accounts receivable management, and elder care industries. He served as Vice President of Acquisitions at Midwest First Financial, Inc. where he was responsible for managing the identification, due diligence, evaluation, acquisition and disposition of performing, sub-performing and non-performing real estate and real estate secured loans. He brings these experiences as well as those from starting, growing and managing his own successful companies to Bot Image™, Inc.
Mr. Manion received his M.B.A. from Creighton University in 1991 and his B.S. in Finance in 1985, also from Creighton University.

Markus Gee
Quality Systems and Regulatory Advisor

Markus Gee | Quality Systems and Regulatory Advisor
Markus has 30+ years of hands-on medical device development, Quality System Management and Regulatory Management experience. This includes building and sustaining certified QMS s, auditing, training facilitation and consultation. He’s been “boots-on-the-ground” in R&D, Product Development, Manufacturing, Regulatory, Quality. Markus has assisted multiple companies in obtaining and sustaining their ISO 13485, MDSAP, CE and MDR Certifications.
Frequently Asked Questions
How often should men get screened for prostate cancer?
The American Cancer Society recommends that men have a chance to make an informed decision with their health care provider about whether to be screened for prostate cancer. The decision should be made after getting information about the possible benefits, risks, and uncertainties of prostate cancer screening. The discussion about screening should take place at:
- Age 50 for men who are at average risk of prostate cancer and are expected to live at least 10 more years
- Age 45 for men at high risk of developing prostate cancer. This includes African American men and men who have a first-degree relative (father or brother) diagnosed with prostate cancer at an early age (younger than age 65).
- Age 40 for men at even higher risk (those with more than one first-degree relative who had prostate cancer at an early age)
After this discussion, men who want to be screened should get the prostate-specific antigen (PSA) blood test. The digital rectal exam (DRE) may also be done as a part of screening. (See Screening Tests for Prostate Cancer.)
If, after this discussion, a man is unable to decide if testing is right for him, the screening decision can be made by the health care provider, who should take into account the man’s general health preferences and values.
If no prostate cancer is found as a result of screening, the time between future screenings depends on the results of the PSA blood test:
- Men who choose to be tested who have a PSA of less than 2.5 ng/mL may only need to be retested every 2 years.
- Screening should be done yearly for men whose PSA level is 2.5 ng/mL or higher.
Because prostate cancer often grows slowly, men without symptoms of prostate cancer who have less than a 10-year life expectancy should not be offered prostate cancer screening, because they aren’t likely to benefit from it. Overall health status, and not age alone, is important when making decisions about screening.
What the American Cancer Society and Medical Community at large do NOT divulge.
- Medical practice evolves very slowly and therefore adoption of new technologies lags the science often by upwards of 10 years.
- PSA has been proven to NOT be effectively correlated with prostate cancer (PCa).
- PSA Velocity or the rate of change of PSA value has some correlation with PCa; therefore, repeat PSA tests periodically (90-180days) is somewhat effective at detecting PCa.
- Many studies over the last five years have shown that non-contrast MRI or bi-parametric MRI (bpMRI) is effective at detection of early stage PCa.
- Most recently, clinical studies conducted by Bot Image, under the prevue of the FDA, have demonstrated the effectiveness of bpMRI aided with artificial intelligence, ProstatID®, in Prostate cancer detection.
Are there any early warning signs of prostate cancer?
Some early warning signs of prostate cancer include urinary and ejaculatory symptoms:
- Urinary symptoms:
- Difficulty starting or stopping urination
- Weak or interrupted urine flow
- Frequent urination, especially at night
- Pain or burning during urination
- Blood in the urine (hematuria)
- Feeling like your bladder isn’t completely empty
- Ejaculatory symptoms:
- Painful ejaculation
- Blood in the semen
- Decreased ejaculate volume
Other symptoms include:
- Trouble getting an erection (erectile dysfunction)
- Pain or stiffness in the lower back, hips, or upper thighs
- Swelling in the lower extremities
However, these symptoms don’t always indicate prostate cancer. For example, many men’s prostates enlarge as they age due to a non-cancerous condition called benign prostate enlargement. If you consistently notice any of these symptoms, you should see your doctor right away and mention the efficacy and non-invasiveness of bi-parametric MRI (bpMRI) in early detection of prostate cancer.
Is it possible to prevent prostate cancer?
There’s no proven prostate cancer prevention strategy. But you may reduce your risk of prostate cancer by making healthy choices, such as exercising and eating a healthy diet.
Prostate cancer is a genetic disease and therefore is more prone to effect men with a family history of the disease. It is important to recognize the symptoms and get effective screening for prostate cancer early such as bi-parametric MRI. What are the different types of screening tests for prostate cancer?
What are the different types of screening tests for prostate cancer?
The two most common screening tests for prostate cancer are the prostate-specific antigen (PSA) blood test and the digital rectal exam (DRE):
PSA blood test
Measures the amount of PSA in your blood. PSA is a protein produced by the prostate gland, and higher levels may indicate prostate cancer. However, a high PSA level isn’t proof of cancer, and the normal range depends on your age. For example, a PSA score above 2.5 ng/ml is considered abnormal for men in their 40s and 50s, while a score above 4.0 ng/ml is considered abnormal for men in their 60s.
DRE
A doctor or nurse inserts a lubricated, gloved finger into your rectum to feel for lumps or other abnormalities in your prostate gland.
If a screening test suggests you might have prostate cancer, your doctor may recommend additional tests, such as a second PSA test or a prostate biopsy
More recently, non-contrast MRI supplemented with AI has shown its efficacy by demonstrating accurate and early detection of prostate cancer; however, due to the cost of a fast MRI (est. $500), many don’t consider this a screening test, but a diagnostic test. Given the significant difference in accuracy of bpMRI plus AI to PSA and DRE, patients may want to consider the additional cost of bpMRI with AI as their choice for screening.
How accurate are screening tests for detecting prostate cancer?
The American Cancer Society and medical community at large recommend PSA testing as the screening methodology; however, multiple scientific studies in the past five years have demonstrated that there is very low correlation between the PSA value and prostate cancer. The accuracy of PSA even with digital rectal exam has been reported at less than 55%; hence, of little value in the end.
We discuss in Question #1 above that bpMRI supplemented by ProstatID artificial intelligence is far more effective at early detection of prostate cancer. With an accuracy at 85% and AUROC or area under the sensitivity-specificity curve of 94%, bpMRI plus ProstatID assists physicians to very accurately detect prostate cancer.
At what age should men start getting screened for prostate cancer?
- Age 50 for men who are at average risk of prostate cancer and are expected to live at least 10 more years
- Age 45 for men at high risk of developing prostate cancer. This includes African American men and men who have a first-degree relative (father or brother) diagnosed with prostate cancer at an early age (younger than age 65).
- Age 40 for men at even higher risk (those with more than one first-degree relative who had prostate cancer at an early age)
Are there any risk factors that increase the chances of developing prostate cancer?
Yes, there are several risk factors that can increase the chances of developing prostate cancer, including:
- Age: The risk of developing prostate cancer increases with age, and most cases are diagnosed in men over 50.
- Race: African American men have the highest rate of prostate cancer.
- Family history: Having a father or brother who developed prostate cancer before age 60, or a close female relative who developed breast cancer, may increase your risk.
- Diet: Eating a high-fat diet, especially one high in red meat or high-fat dairy products, may increase your risk.
- Obesity: Being at a higher weight may increase your risk.
Other risk factors include: Inherited faulty genes, Hormone levels, and Pesticides.
How do doctors determine the stage and aggressiveness of prostate cancer?
Doctors use multiple factors to determine the stage and aggressiveness of prostate cancer, including:
- PSA blood test
A protein produced by the prostate, higher levels of PSA can indicate more advanced cancer. Doctors also consider how quickly PSA levels have been increasing, as a faster increase could indicate a more aggressive tumor.
- Prostate biopsy
A test that removes tumor tissue and can indicate how much of the prostate is involved and the Gleason score. The Gleason score is a number between 2 and 10 that describes how cancer cells look under a microscope and how quickly they can grow and affect other tissue. A higher score indicates a more aggressive cancer that is more likely to spread quickly.
- Imaging tests
These tests can also be used for initial staging.
- Tumor, Nodes and Metastasis (TNM) staging system
This system measures how far prostate cancer has spread in the body, with the T score rating the size and extent of the original tumor. The most widely used TNM system for prostate cancer is the AJCC (American Joint Committee on Cancer) TNM system, which was most recently updated in 2018.
Are there any alternative or complementary tools for diagnosis for prostate cancer?
Yes, bi-parametric or multi-parametric MRI aided by artificial intelligence (AI) has demonstrated significant improvement over non-AI aided MRI in detection and diagnosis of prostate cancer.
In clinical studies involving a dozen physician specialists (radiologists board-certified in abdominal MRI), the AI software, ProstatID demonstrated a 20 point improvement (100 point scale of sensitivity-specificity) in detection and diagnosis over the participating physicians reading 150 MRI cases from various MRI systems produced by the leading manufacturers; Siemens, Philips and GE.

