We Get You.
You’re busy, you’re overwhelmed trying to keep up with new studies, pharmaceuticals, protocols and processes, and medical devices. We also observe that the NCCN guidelines are always many years behind the rapidly evolving technologies. Our mission is to spare your time, improve your clinical performance and patient outcome, and provide you with adequate information and fact to justify changes in your practice.

Our focus is on the patient and their Prostate Cancer detection and diagnosis.
And with our unique FDA clearance, we also offer Screening for Prostate cancer using non-contrast MRI aided by our AI algorithm, ProstatID.
We offer time and cost-savings to you and the patient.
This requires only a 15-20 minute MRI and results are generated within minutes and populated on the radiological server and workstations.

ProstatID offers significant performance improvements in detection and reduction of false positives.
Read more about our clinical studies involving 25 US board-certified radiologists
Benefits For Imaging Centers, PCPs and Urologists
ProstatID offers you a significant boost in diagnostic confidence non-invasively
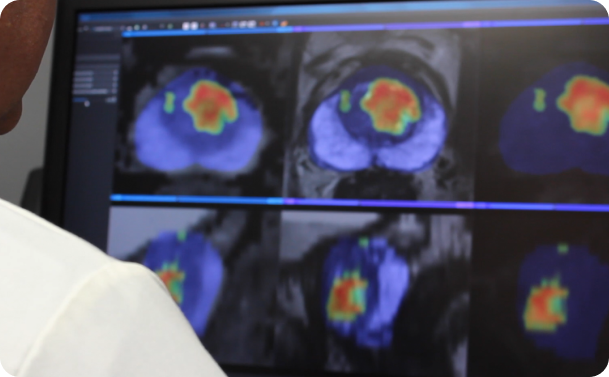
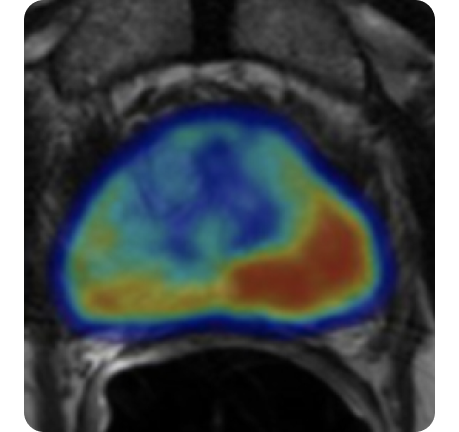
The AI software output provides an excellent 2D and 3D visual representation (as shown in the figures below) as to the location and size of suspicious lesions for patient discussions and treatment planning – including doing nothing except waiting and watching – active surveillance.

And further, with our powerful tool, you are providing the bridge from diagnosis to treatment, if treatment is necessary.
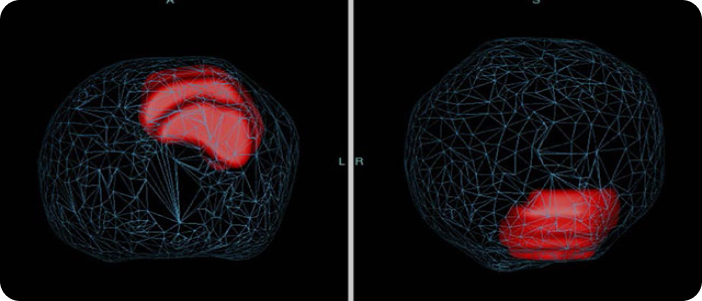
The images below indicate a 2D and corresponding 3D views of the prostate in mesh with the cancerous lesion size and location (in red) within the prostate from two viewpoints useful for cognitive biopsy and/or treatment planning.
ProstatID requires no contrast injection, saving MRI scanning time, reducing patient risk, reducing overall costs to both provider and patient, all while improving patient outcome.
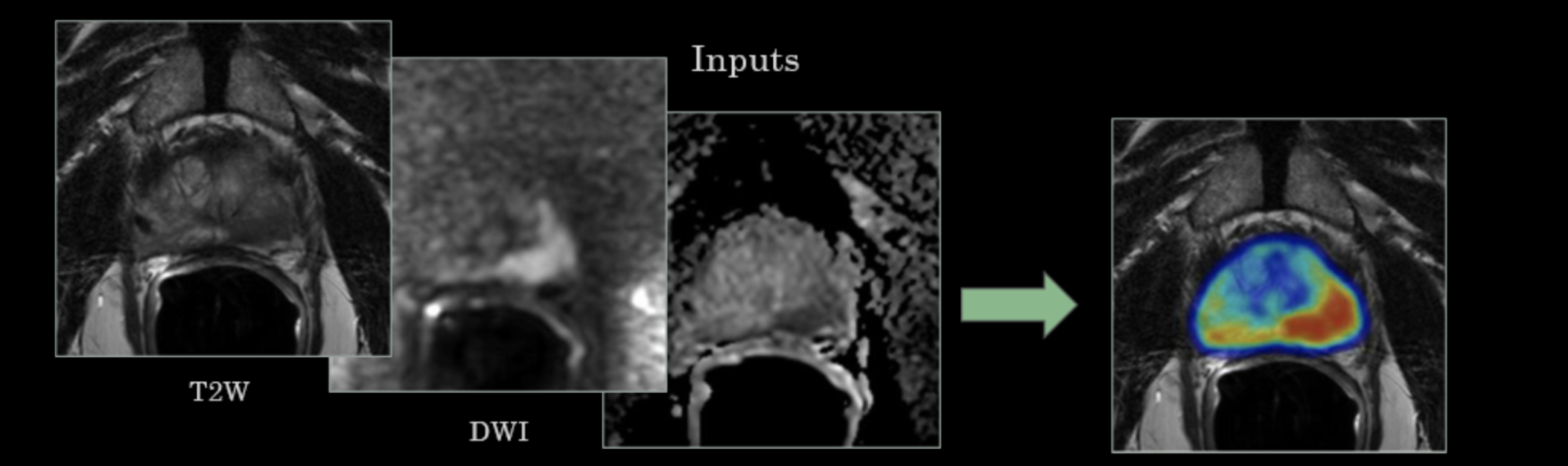
User sends or pushes the requisite to provide the requisite three input MRI series in order to generate a copy of one series with a colorized overlay indicating the margins of each and every suspicious lesion within the organ, along with its cancer-risk score. A full DICOM compatible PDF report is also included.
How ProstatID Works
Scan
Technologist performs standard screening or diagnostic MRI sequences and pushes the study to their PACs with is Standard Operating Procedure. In parallel, they push the study to the Platform partner of cloud service provider.

Detect
ProstatID automatically detects study, sorts for necessary sequences, checks quality, performs the detection and diagnosis and returns an appended series to the unique patient ID with results and report to view in less than 5 minutes typically = real-time diagnosis.

Diagnose
This new series and report are appended to the study so that the radiologist sees it along with all others on his/her viewing station; hence, no additional effort, equipment or work to perform.

Treat or
Don’t Treat
ProstatID assists physicians with treatment planning by providing an entire view of the organ highlighting all suspicious lesions with their individual risk scores. Additionally, if lesion(s) are graded as high risk, they are presented in two powerful 3D views within a transparent rendition of the prostate gland giving interventionalists ideal cognitive targeting.

It takes a village to change things and following the academic papers and science demands time that few have.
See our “references section” to support the growing hypothesis that patients benefit from an MRI prior to biopsies – this, despite slow adaptation from the insurance industry, is the best medicine.
For MRI providers
This low-cost per click service is available now with as little as an hour time of your IT department.
For PCPs
Ask your MRI provider to add-on ProstatID AI to gain the beneficial impact of this software, or ask us for a MRI provider near you.
For Urologists
This software provides a whole-organ view of and 3D roadmap of the organ that has proven to be an excellent tool for cognitive biopsy or treatment guidance.
Let us demonstrate to you how effective and accurate our prostate cancer detection diagnosis and screening software is for improving your efficiency and patient care.
Contact us below and see how easy it is to get your facility connected via secure VPN to Bot Image™'s ProstatID.
Learn more about our Prostate Centers of Excellence and Concierge Medicine Coalition where you and your patient benefit from the highest quality care methodologies and technological improvements.
Frequently Asked Questions
What is AI and how is it used in diagnosing prostate cancer?
Artificial intelligence is the science of making machines that can think like humans. It can do things that are considered “smart.” AI technology can process large amounts of data in ways, unlike humans. The goal for AI is to be able to do things such as recognize patterns, make decisions, and judge like humans refers to software that has been. Artificial Intelligence software used in diagnosing prostate cancer using MRI has been trained on large quantities of prostate MRI data also containing localized data points within that have been validated by biopsy and pathology labs indicated the grade of cancer if it exists at those points. This training then facilitates the software to recognize cancer better than can be detected by trained humans due to the many features that the software uses versus those few features visible with the human eye.
Artificial intelligence (AI) can help diagnose prostate cancer in several ways, including:
- Treatment guidance
AI can help identify the extent of a tumor, predict its location, and review MRIs. For example, the machine learning algorithm ProstatID® has been used in clinical trials to increase tumor detection and extent identification as well as provide three dimensional targeting useful for interventionalists in cognitive fusion targeting.
- Computer-assisted diagnosis
AI software can help pathologists detect, grade, and measure tumors in prostate biopsies. For example, Oxford University Hospitals (OUH) NHS Foundation Trust is trialing Paige Prostate, an AI software that helps pathologists read biopsy slides, flag suspicious areas, and assess tumor aggressiveness.
- Non-invasive imaging
AI models can help detect and characterize cancer aggressiveness in non-invasive radiology images like MRIs and ultrasounds. AI can also help with tasks like prostate gland segmentation and MRI-ultrasound registration. The AI product, ProstatID has demonstrated the ability to detect, diagnosis, segment (outline) suspicious tumors and classify (risk stratify) them with non-invasive, non-contrast MR Imaging.
AI can help with risk stratification and patient monitoring. AI tools can access a larger databases of knowledge than humans, and can scan extract and detect far more properties and nuances within the images that the human eye is capable of.
Can AI accurately detect and diagnose prostate cancer?
The Food and Drug Administration has approved AI-assisted tools to help detect cancers of the brain, breast, lung, prostate, skin, and thyroid. Recent and ongoing studies show promising results for additional tools.
Furthermore, AI has shown promise in improving the specificity and standardization of prostate cancer diagnosis and mitigating the risk of unnecessary biopsies.
ProstatID, for example has been FDA cleared as an aid for detection, diagnosis, screening and classification of prostate cancer.
How does AI differ from traditional methods of diagnosis for prostate cancer?
AI models can help in detecting and characterizing cancer aggressiveness on non-invasive radiology images (MRI and ultrasound), serving physicians by assisting them in improving their interpretation performance or accuracy. It does this by having been trained on large quantities of data from previous clinical images and specimens.
Are there any limitations or drawbacks to using AI for prostate cancer diagnosis?
Limitations to using AI for prostate cancer diagnosis include the following:
- Not all AI are the same, in fact, all offer different outputs and services and are adapted to limited number of MRI systems; therefore, physicians should do their homework to differentiate those systems and understand their limitations, functions, outputs and performance.
- Those limitations associated with patients not suitable for MRI such as those with pacemakers, or certain metallic implants – part of the screening process prior to obtaining an MRI.
- Possible limitations as to which MRI systems that the AI has been trained and cleared for use with. For example, ProstatID has been trained on MRI platforms of GE, Siemens and Philips with others in-works.
- Possibly Patients with metallic hip replacements – this typically renders 3 Tesla MRI useless in scanning prostates; therefore, the AI cannot process this data
- Possibly Patients for whom their prostate has been removed.
- The AI may not be intended for patients who have undergone or are currently undergoing various treatments in the prostate including active chemotherapy, radiation therapy, radio frequency ablation, or other prostate or cancer treatments.
- AI is typically an adjunctive tool and not intended to replace a physicians’ own review of a prostate MRI.
- Decisions should not be made solely based on analysis by AI.
- The AI device likely should not be used on patients who have used antiandrogens and/or LHRH within the past 6 months and 12 months respectively.
- The AI device likely should not be used on patients having undergone prostate biopsies within 8-12 weeks unless the MRI is clinically indicated by the physician.
There are no reported drawbacks to utilization of AI for prostate cancer diagnosis other than cautionary publications regarding the qualification of AI and understanding of its limitations and performance criteria by physicians prior to their using it.
Does the use of AI in prostate cancer diagnosis require additional training or resources for doctors?
AI vendors must provide users manuals and offer training to physicians utilizing the software. Given that AI products considerably differ in functionality, performance, and limitations, physicians should understand these prior to use.
Some, such as ProstatID, require no installation, nor additional hardware, or manual operations; hence, very little training in its use is required. Its outputs are directed back to the original sender and unique patient ID without any physician involvement.
Is Prostate AI accessible to all patients regardless of their location or healthcare provider?
Yes; however, patients must first obtain a prostate MRI from a compatible MRI system (see Limitations question #13), and also request from their provider an AI assisted interpretation. Many MRI facilities may not offer such AI services, but these can be accessed by the patient requesting this from the provider or obtaining a copy of the MRI and contracting a concierge physician to send them to the AI service provider.
A second opinion MRI interpretation by an FDA cleared prostate MRI software such as ProstatID is encouraged especially if symptoms persist after previous MRIs and/or biopsies.
Insurance reimbursement remains an issue in the US, but fortunately, ProstatID offers the unique 3D output to assist in detection and diagnosis; thereby, meeting the requirements to utilize that specific CPT reimbursement code. Contact Bot Image, Inc. for additional information.
How do privacy concerns play a role in the use of AI for prostate cancer diagnosis?
AI may or may not utilize PHI or protected health information, and if the PHI is recorded and saved, the AI provider must comply with HIPAA requirements. Prostate AI such as ProstatID does not utilize PHI; only the anonymized MRI image sets; hence, there are no privacy concerns regarding its use.
Are there any past or ongoing studies or research on the effectiveness of AI in detecting and diagnosing prostate cancer?
Bot Image, Inc. conducted two clinical studies involving 25 physicians and 300 prostate MRI cases over two years and reported results to the FDA via the 510(k) process. The results exceeded the FDA threshold of demonstrating statistically significant improvement in reader performance of interpreting prostate MRIs and detecting and diagnosing prostate cancer.
More recently, several additional independent studies have demonstrated the superiority of AI over human readers interpreting prostate MRI such as below.
AI System Beats Radiologists in Detecting Clinically Significant Prostate Cancer— AI detected 6.8% more clinically significant cancers, 20% fewer indolent cancers from https://www.medpagetoday.com/radiology/diagnosticradiology/110635. An international study led by Radboud University Medical Center compares and assesses AI with clinical outcomes and radiologist assessments. It finds that AI is more accurate than radiologists in detecting prostate cancer and reduces the frequency of false alarms by half. These findings are published in The Lancet Oncology.
AI detects cancer with 17% more accuracy than doctors: UCLA study concludes: A new study from UCLA found that an AI tool identified prostate cancer with 84% accuracy — compared to 67% accuracy for cases detected by physicians, according to a press release from the university.
Applications of Artificial Intelligence in Prostate Cancer Care: A Path to Enhanced Efficiency and Outcomes https://ascopubs.org/doi/10.1200/EDBK_438516#:~:text=Several%20registered%20clinical%20studies%20are,prospective%20insights%20(Table%201). This paper lists a table of ongoing studies utilizing AI.
How does AI assist in determining the stage and aggressiveness of prostate cancer?
Firstly, AI models such as ProstatID properly trained to detect, segment and classify suspect lesions yield improvements in early detection of aggressive disease. They are able to perform these tasks through training deep learning and/or random forest models algorithms using large amounts of MRIs with their three-dimensionally localized biopsies and associated pathology reports. Through training, the software can then distinguish between clinically significant cancer and indolent or false cancers such as Gleason grade 6 cancers with a high degree of accuracy (see #17 above).
Secondly, AI also assists pathologists in better interpreting histologic specimens from biopsies and identifying and classifying various grades of cancers. https://blog.google/technology/health/using-ai-identify-aggressiveness-prostate-cancer/
Is AI being integrated into routine prostate cancer screenings and diagnosis procedures?
Unfortunately, both MRI and AI are not yet widely adapted nor routinely implemented despite the significant evidence presented in the industry and academic forums. As mentioned previously, changes in medical practice and insurance industry happens very slowly; hence, an informed patient that has access to knowledge and improved technologies can significantly improve their clinical outcomes.
Using bpMRI with AI for screening has demonstrated a clinically and statistically significant improvement over the current standard of care of PSA monitoring and biopsies without aid of MRI and AI driven targeting.
Are there any cost differences between traditional methods and using AI for prostate cancer diagnosis?
Cancer diagnosis typically concludes with biopsy confirmation of a positive MRI, and this billing and payment process is well established with CPT codes within the insurance industry. The added costs of using AI vary based upon the AI company and services provided. There exists offsetting revenues from the use of some AI by proven CPT codes for such services as 3D reconstruction for use in detection and diagnosis as provided by ProstatID for example in which the revenues exceed the added costs.
How is accuracy measured when it comes to using AI for diagnosing prostate cancer?
In AI prediction, accuracy is a metric that measures how often a machine learning model correctly predicts an outcome. It’s calculated by dividing the number of correct predictions by the total number of predictions, and is often represented as a percentage or value between 0 and 1. A higher accuracy is better, with a perfect accuracy of 1.0 meaning the model is correct every time. Statistically, this is the number of true positive and true negatives divided by the total number of true and false positive and negatives (these four equal the confidence matrix) or total predictions. Most trained physicians score around 0.70 while AI should perform significantly better in order to have positive impact.
Alternatively, measuring the sensitivity-specificity performance using the same confidence matrix yields the area under the receiver operating curve or AUROC of sensitivity-specificity which weighs the trade-offs of sensitivity at detection of true positives to false negatives to the specificity of detecting true cancers from false positives. Again, a perfect score is 1 or 100%, and in clinical studies conducted by Bot Image regarding ProstatID performance, its standalone AUROC was 93.6% compared to a high of 74.0% achieved by a participating radiologist.
Are there any concerns about relying solely on AI for prostate cancer diagnosis without human oversight?
Of course, even in today’s technological world of advancements, AI is not completely relied upon without human oversight in medical diagnostics such as prostate cancer diagnosis. The FDA and other countries’ regulatory bodies have not cleared AI for use without a trained physician using/overseeing its use. Even if the software has proven superior to trained physicians in clinical studies, the software has not been trained and likely could not be trained for every conceivable deviation that may occur in the course of use.

