Overview: ProstatIDTM is North America’s first FDA-Cleared Prostate Cancer SCREENING, Detection and Diagnostic AI software. With 94% AUROC (Area under the Receiver Operating Curve of sensitivity-specificity), physicians can reliably detect and diagnose prostate cancer from MRI in far less interpretation time, with much higher confidence, and significantly improve their positive detection while decreasing false positives. More importantly, this same algorithm can disrupt the industry by providing a very accurate and cost-effective means for early detection via a 20-minute MRI saving the healthcare industry billions (USD) in unwarranted biopsies and procedures from false-positives, missed and late detections that result in even more expensive treatments. MRI with ProstatID is destined to become the new Standard of Care similar to what colonoscopy was years ago.
Probing Questions & Pain Points:
Pertinent Facts:
- Prostate Cancer (PCa) is the 3rd leading cause of death amongst men in North America – behind lung cancer and heart disease.
- Prostate Cancer is relatively slow growing and typically can be detected early
- Early detection is dependent upon men over 50 getting annual blood tests such as PSA. Elevated PSA (over 4ng/ml) are indicators of something wrong in the prostate; however, not correlated with cancer, it does often result in further testing such as MRI.
- MRI has proven to be the most effective diagnostic tool for PCa detection AND localization.
- There are two forms of MRI studies, one, multi-parametric MRI (mpMRI) uses contrast agents injected into the blood stream with real-time dynamic contrast enhancement (DCE) and the other, bi-parametric MRI (bpMRI), does not; therefore bpMRI is much faster and more cost effective. However, mpMRI today is indicated for diagnosing prostate cancer in post-treated prostates. Then again, literature has demonstrated that bpMRI has proven over 99% as effective as mpMRI when read by a panel of expert radiologists2,3. These references did not take into account the use of AI to further improve the diagnostic accuracy using bpMRI as they preceded all such AI developments.
- In contrast, expensive blood tests looking at other genetic markers may perform well at confirming prostate cancer, but ad little value in determining how serious or the location of lesion(s); hence, don’t contribute to the treatment planning.
- Urologists however, hold tight to their belief in Random 12-core or TRUS guided biopsies while exhibiting slow adaptation to utilizing MRI.
- Radiologists have performed poorly for many years and contributed to the urologist’s skepticism; and they discuss this in forums out of the public view. Only the most highly trained and experienced perform at the level described in the NIH article above.
Pain Points:
- Interpreting Prostate MRI is very challenging and increases when the patient has other conditions such as BPH (Benign Prostate Hyperplasia), Prostatitis, cysts, etc.
- “Reading Prostate MRI is time-consuming while searching through stacks of 20-30 slices while simultaneously viewing corresponding slices of multiple series (ie, T2W Axial, DWI, ADC) and cross-checking Coronal and Sagittal Views of T2W.
Solutions:
- ProstatID requires no additional steps, buttons, or firmware operation as it automatically appends its results to the patient study after the MRI tech has “pushed” the study to their PACs and AI Platform provider.
- ProstatID returns the detection and diagnostic results back to the sender typically in less than 5 minutes; hence, the attending physician can begin reading the study while the patient remains on the MRI table; thus, real-time diagnostic assistance.
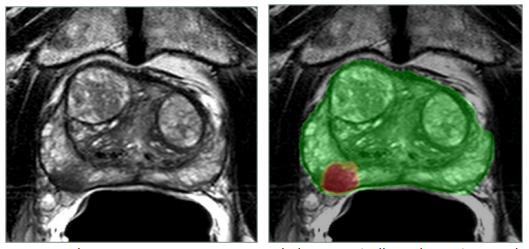
- ProstatID returns a colorized “heat map” or probability map overlayed on a copy of the T2W image as shown below where red is high probability of cancer and green is normal or benign tissue. This facilitates very rapid interpretation as physicians can focus on the few yellow (medium suspicion) and red spots and chose to agree or disagree and dictate their report.
- ProstatID also returns a PDF report appended automatically to the patient study. This includes axial views such as above of each and every suspicious lesion; the exact 3D location, size, and border (segmentation) of each lesion as well as it’s probability score.
- ProstatID report also includes the volume of the prostate so that the physician doesn’t have to manually measure and calculate it (with typically poor accuracy as a prostate is irregularly shaped and not the Prolate Ellipse mathematical formula used in the calculation by measurements on the image: prolate ellipse volume (cm)=(length×width×height)×π/6. Thus, time and accuracy improvements yield more accurate PSA density calculation (free PSA/volume) which are more correlated to PCa.
- ProstatID also offers a PI-RADs case score and 3D rendition of the prostate organ with suspicious 3D lesions inside a transparent mesh for precise localization and treatment planning.
Clinical Validation & Value based metrics:
- ProstatID started with the premise provided by it’s prototype created by the NIH4. They proved the utility of AI for improving PCa detection and classification.
- Two clinical studies were conducted in 2020 and 2021 involving a total of 25 radiologist of varying training and experience levels interpreting PCa. These data were used to apply for and obtain FDA-clearance and are being used to obtain the CE-mark for EU (forthcoming).
- Various beta test sites have conducted their own internal studies and provided testimonials as to how well the software works. Testimonials follow below.
- Proven reduction of unnecessary biopsies as a result of reduction of false positives by over 30% and proven PCa detection improvement of greater than 6.6% over industry leading radiologists – up to 25% over non-seasoned experts.
- Proven reduction of radiologists’ read time from 20-30 minutes per case to around 5 minutes per case or roughly 200% reduction.
- Two peer reviewed articles5,6 have been published regarding thus far indicating the superiority of the algorithm and its effectiveness.
- Most recent article published in the UK7 states the effectiveness of bpMRI as a prostate cancer screening tool (see hyperlink below).
Testimonials:
- Dr. Lynch: “I use ProstatID on every case. I first look at all of the colorized suspect lesions, then study them and make my diagnosis. Usually, I follow ProstatID 100%”. He later exclaimed “ProstatID has been right-on with biopsy confirmation”.
- “We are on board with ProstatID. I feel more comfortable with AI backing me up.” Dr. Chris Woodhouse, MD
- “I’ve known Randy {Dr. Randall Jones, founder of Bot Image, Inc. and co-inventor of ProstatID} as a friend, a patient-advocate, and, yes-as a nerdy physicist. His ingenuity and eye for the future are only matched by his unflagging support for the health of humanity. This Software gives us a glimpse of how empathy and technology can collide for the good of us all.”
Eric Walser MD
John Sealy Professor and Chairman of Radiology
The University of Texas Medical Branch
Galveston, Texas
Typical Clinical Workflow & ProstatID’s impact: - Technologist performs standard screening or diagnostic MRI sequences and pushes the study to their PACs with is Standard Operating Procedure. In parallel, they push to the Terarecon Platform (if not automated by Terarecon).
- ProstatID automatically detects study, sorts for necessary sequences, checks quality, performs the detection and diagnosis and returns an appended series to the unique patient ID with results and report to view in less than 5 minutes typically – real-time diagnosis.
- This new series and report are appended to the study so that the radiologist sees it along with all others on his/her viewing station; hence, no additional effort, equipment or work to perform.
References and Peer Reviewed Articles (w/highlights):
- https://www.ncbi.nlm.nih.gov › articles › PMC8988779 MRI has good diagnostic accuracy for clinically significant prostate cancer. A PI-RADS 2 or lower finding has a negative predictive value of 96% for clinically significant cancer, and a PI‐RADS 3, 4 or 5 MRI scan has a sensitivity of 93%.
- Assessment of the Diagnostic Accuracy of Biparametric Magnetic Resonance Imaging for Prostate Cancer in Biopsy-Naive Men, The Biparametric MRI for Detection of Prostate Cancer (BIDOC) StudyMore bpMRI, Lars Boesen, MD, PhD1; Nis Nørgaard, MD1 ; Vibeke Løgager, MD2; et al, JAMA Netw Open. 2018;1(2):e180219. doi:10.1001/jamanetworkopen.2018.0219 Conclusions and Relevance: Low-suspicion bpMRI has a high NPV {97%} in ruling out significant prostate cancer in biopsy-naive men. Using a simple and rapid bpMRI method as a triage test seems to improve risk stratification and may be used to exclude aggressive disease and avoid unnecessary biopsies with its inherent risks. Future studies are needed to fully explore its role in clinical prostate cancer management.
- Clinically Significant Prostate Cancer Detection With Biparametric MRI: A Systematic Review and Meta-Analysis, Renato Cuocolo, MD1, Francesco Verde, MD1, Andrea Ponsiglione, MD1, Valeria Romeo, MD, PhD1, Mario Petretta, MD2, Massimo Imbriaco, MD1 and Arnaldo Stanzione, MD1, American Journal of Roentgenology. 2021;216: 608- 621. 10.2214/AJR.20.23219Conclusion: Results confirm the feasibility of bpMRI for the detection of csPCa and for reducing acquisition time, patient discomfort, and costs. Nevertheless, the available studies proved to be heterogeneous, indicating a need for a more robust validation of this imaging protocol and a standardization of prostate bpMRI acquisition and reporting.
- NIH – ProstatID’s beginnings: Detection of prostate cancer in multiparametric MRI using random forest with instance weighting, Nathan Lay,a Yohannes Tsehay,a Matthew D. Greer,b Baris Turkbey,b Jin Tae Kwak,c Peter L. Choyke,b Peter Pinto,b Bradford J. Wood,c and Ronald M. Summers,a, Journal of Medical Imaging 4(2), 024506 (Apr–Jun 2017). *a: National Institutes of Health, Clinical Center, Imaging Biomarkers and Computer Aided Diagnosis Laboratory, Bethesda, Maryland, United States; b: National Institutes of Health, National Cancer Institute, Urologic Oncology Branch and Molecular Imaging Program, Bethesda, Maryland, United States; c, National Institutes of Health, Clinical Center, Center for Interventional Oncology, Bethesda, Maryland, United States.Conclusion: The random forest, features, sampling strategy, and instance-level weighting improve prostate cancer detection performance [area under the curve (AUC) 0.93] in comparison to SVM {earlier CAD method} (AUC 0.86) on the same test data.
- Comparison of machine learning methods for detection of prostate cancer using bpMRI radiomics features, Ethan J Ulrich1 , Jasser Dhaouadi1, Robben Schat2, Benjamin Spilseth2, and Randall Jones1, Book of Abstracts, ISMRM Annual Meeting, London, UK, May 2022. Conclusion Regarding BotImage’s ProstatID: While all models demonstrated similar performance when evaluating at the lesion-level (ROC analysis), bpRF outperforms other models on FROC analysis. This indicates that the bpRF model produced fewer false positive detections at equal sensitivity. This comparison was done with traditional Neural Net and other algorithms published recently. The ProstatID detection engine is superior.
- Improving Prostate Cancer Detection with MRI: A Multi-Reader, Multi-Case Study Using Computer-Aided Detection (CAD), Mark A. Anderson, MD*, Sarah Mercaldo, PhD*, Ryan Chung, MD, Ethan Ulrich, BS, Randall W. Jones, PhD, MBA, Mukesh Harisinghani, MD*, Academic Radiology 2022, https://doi.org/10.1016/j.acra.2022.09.009 * Dept. of Radiology, Mass General Hospital.Conclusion Regarding BotImage’s ProstatID: Addition of a random forest method-based {ProstatID}, CAD-generated MRI image series improved inter-reader agreement and diagnostic performance for detection of clinically significant prostate cancer, particularly in the transition zone.
- Prostate Cancer Treatment can be safely delayed, and inexpensively and accurately monitored thanks to new Artificial Intelligence (prnewswire.com)
- A narrative review of biparametric MRI (bpMRI) implementation on screening, detection, and the overall accuracy for prostate cancer, Greenberg, Koller, Casado, Triche, Krane, Ther Adv Urol, 2022 May 4. Doi 10.1177/17562872221096377. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9073105/#:~:text=These%20meta%2 Danalyses%20highlight%20bpMRI,RADS%20v2%20score%20into%20account.


