
Blog
Prostate MRI is a powerful diagnostic tool, offering a detailed view inside the body to help physicians find and assess potential cancers. However, the quality of these images can sometimes be affected by “artifacts.” These are distortions or errors caused by factors like patient motion, hardware limitations, and normal bodily functions. For accurate prostate cancer lesion detection and classification, understanding and correcting these artifacts is essential. Clean, clear images are the foundation of a confident diagnosis, whether read by a radiologist or analyzed by an AI system.
Understanding MRI Artifacts in Prostate Imaging
To appreciate the importance of high-quality imaging, we first need to understand what can go wrong. Artifacts are the unwanted guests in an MRI scan, and managing them is a critical part of the diagnostic process.
What are MRI artifacts?
In simple terms, MRI artifacts are distortions or errors in the final images that do not represent the actual anatomy of the patient. They can appear as blurring, ghost-like images, bright or dark spots, or geometric distortions. Think of it like taking a photo with a shaky hand or a smudged lens—the resulting picture isn’t a true representation of the subject. These flaws can obscure important details or, worse, create false ones.
Why artifacts matter in prostate MRI
In prostate imaging, precision is everything. The prostate is a small gland, and cancerous lesions can be even smaller. Even minor distortions can have significant consequences. Artifacts can lead to the misclassification of lesions, making a benign area look suspicious or hiding a clinically significant cancer. This reduces a radiologist’s diagnostic confidence and can lead to false positives, causing unnecessary anxiety and follow-up procedures, or false negatives, which delay critical treatment. For any diagnostic pathway, minimizing MRI artifacts in prostate imaging is a non-negotiable first step.
Common Sources and Types of Artifacts in Prostate MRI
Artifacts arise from several sources, including the patient, the MRI hardware, and the physics of the imaging process itself. Understanding these sources helps technologists and radiologists anticipate and mitigate them.
Patient motion and physiological movement
The single biggest challenge in MRI is patient movement. An MRI scan can take a considerable amount of time, and even small, involuntary movements can create artifacts. In prostate MRI, breathing and bowel peristalsis (the natural movement of the intestines) are major culprits. This motion is particularly disruptive to diffusion-weighted imaging (DWI) sequences, which are highly sensitive to movement and crucial for identifying cancerous tissue.
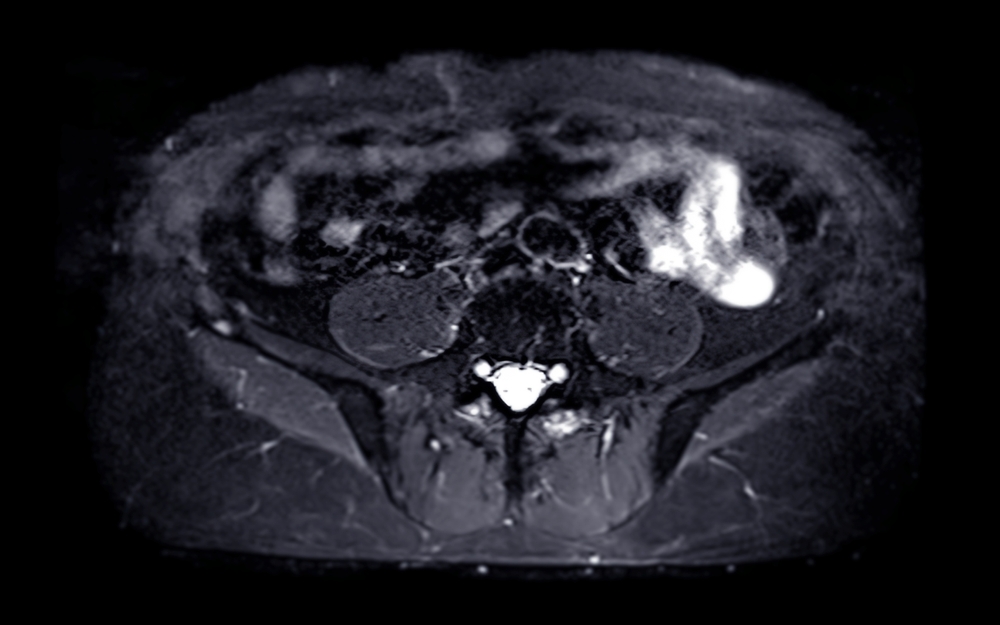
Magnetic susceptibility and distortion artifacts
Magnetic susceptibility artifacts occur when different materials within the scanner’s magnetic field interact with it differently. A common cause in prostate imaging is rectal gas. The air in the rectum distorts the magnetic field, which can warp the shape of the prostate on the image, creating a significant prostate MRI distortion. Metallic implants, such as hip prostheses, are another major source of susceptibility artifacts, creating large black voids and distortions that can completely obscure nearby anatomy.
Gibbs ringing and chemical shift artifacts
Gibbs ringing, also known as a truncation artifact, appears as fine parallel lines near sharp intensity boundaries, like the edge of the prostate capsule. It can sometimes be mistaken for a capsular breach. Chemical shift artifacts, on the other hand, result from the different resonant frequencies of fat and water molecules. It often manifests as a dark or bright band at fat-water interfaces, which can complicate the evaluation of the prostate’s margins. These are commonly seen in both T2-weighted and DWI images.
RF inhomogeneity and field non-uniformity
An ideal MRI requires a perfectly uniform magnetic field and radiofrequency (RF) pulse application. In reality, imperfections exist. RF inhomogeneity can cause signal dropouts or uneven brightness across the image, meaning one part of the prostate may appear darker than another for purely technical reasons. This is more common with certain coil setups, like endorectal coils or when using multi-channel surface coils without proper calibration, and can make lesion detection unreliable.
Artifact Impact on Prostate Cancer Lesion Detection
Artifacts are not just minor annoyances; they directly interfere with the diagnostic process, affecting human interpretation and artificial intelligence models alike.
Diagnostic pitfalls due to artifacts
Artifacts can create a minefield of diagnostic challenges. Motion can blur the margins of a lesion, making it difficult to assess its size and relationship to surrounding structures. Susceptibility artifacts from rectal gas can compress or distort the peripheral zone, where most prostate cancers occur. Perhaps most dangerously, some artifacts can mimic lesions. For example, a flow artifact from a blood vessel could be mistaken for an enhancing tumor on contrast-enhanced images, while distortions on ADC maps can create false low-signal areas that look like cancer.
Artifact effects on PI-RADS scoring
The Prostate Imaging-Reporting and Data System (PI-RADS) is a standardized system for scoring the likelihood of clinically significant prostate cancer based on MRI findings. This scoring relies heavily on the clear visualization of features in T2-weighted, diffusion-weighted, and dynamic contrast-enhanced sequences. Artifacts can directly degrade the image quality of these key sequences, leading to inaccurate PI-RADS scores. A motion-blurred DWI, for instance, might prevent a confident assessment, leading to an indeterminate score and diagnostic uncertainty.
Influence on AI-based classification
Artificial intelligence models, like Bot Image’s ProstatID™, are trained on vast datasets of high-quality images to recognize the subtle patterns of cancer. When these models are fed images with significant artifacts, their performance can suffer. Image distortions can confuse the AI, leading to less reliable classifications. Just as a human expert needs a clear view, an AI algorithm’s accuracy depends on clean, artifact-free data. Therefore, robust image correction methods are vital for the successful implementation of AI in clinical practice.
Artifact Reduction and Correction Strategies
Fortunately, a combination of careful preparation, technical optimization, and advanced software can significantly reduce or correct artifacts. This multi-pronged approach ensures the highest possible image quality.
Pre-scan preparation and patient setup
Quality starts before the scan even begins. Simple preparations can make a huge difference. Patients may be advised to empty their rectum before the scan to minimize rectal gas. In some cases, a mild, temporary antiperistaltic agent may be administered to reduce bowel motion. Clear communication with the patient, explaining the importance of remaining still, and making them as comfortable as possible can also drastically reduce motion-related artifacts.
Hardware and acquisition optimization
Technologists play a key role in optimizing the scan protocol. Using a scanner with strong gradients and excellent field homogeneity provides a better foundation for high-quality images. Techniques like parallel imaging (which speeds up scans) or using high-bandwidth sequences can reduce certain types of artifacts like chemical shift. Careful planning of the imaging slices to avoid known sources of distortion, when possible, is also a critical step.
Post-processing and software-based correction
When artifacts cannot be prevented, they can often be corrected with software. Modern imaging platforms include sophisticated distortion correction algorithms that can mathematically “unwarp” images affected by magnetic field inhomogeneity. Non-rigid registration algorithms can align images from different sequences (like T2 and DWI) that have been misaligned by patient motion. Furthermore, emerging AI-based tools can identify and suppress artifacts, effectively cleaning up the images before they are presented to the radiologist.
Best Practices for Minimizing Artifacts in Key Sequences
Different MRI sequences are susceptible to different types of artifacts. Applying specific strategies for each one is essential for a comprehensive, high-quality prostate exam.
T2-weighted imaging (T2WI)
T2-weighted images provide the anatomical foundation for prostate MRI. To ensure crisp images, technologists often use techniques to reduce ghosting from breathing and bowel motion. This can involve adding “saturation bands” that nullify the signal from moving structures outside the prostate. Optimizing the number of signal averages can also improve the signal-to-noise ratio, providing clearer edge detail for better assessment of the prostate capsule.
Diffusion-weighted imaging (DWI) and ADC maps
DWI is extremely sensitive to motion and distortion. To combat this, faster DWI sequences are often preferred. It is also crucial to apply geometric distortion correction algorithms, especially when comparing the DWI series to the T2-weighted images. The choice of b-values—which control the degree of diffusion weighting—is also important. A proper selection helps maximize the contrast between cancerous and healthy tissue while minimizing noise.
Dynamic contrast-enhanced (DCE) MRI
DCE MRI involves acquiring images rapidly after a contrast agent is injected. Patient motion during this phase can make it impossible to accurately analyze how tissue enhances over time. Motion correction algorithms are therefore essential. These software tools register, or align, each time-resolved image to a reference scan, ensuring that any changes seen are due to contrast uptake, not patient movement.
Advanced Correction Methods and Future Directions
The field of MRI is constantly evolving, with new hardware and software technologies promising even better solutions for artifact correction.
AI-driven artifact correction and reconstruction
One of the most exciting frontiers is the use of AI for artifact suppression. Deep learning models can be trained to recognize the patterns of specific artifacts—like motion or noise—and subtract them from the image data. Some models can even reconstruct a clean image from corrupted or undersampled data, potentially leading to faster scans with higher quality. These real-time AI image correction methods are poised to become a standard feature in future MRI systems.
Prospective motion correction technologies
Instead of correcting for motion after the fact, prospective motion correction aims to prevent it from ever degrading the image. This involves using real-time tracking systems, such as small sensors or camera-based navigators, that detect patient movement as it happens. This information is fed back to the scanner, which instantly adjusts the imaging parameters to compensate for the motion, effectively freezing the anatomy in place.
Harmonization across scanners and protocols
A major challenge in multi-center studies and AI model development is variability in image quality between different MRI scanners and protocols. Harmonization is the process of standardizing image acquisition and applying correction techniques consistently to ensure that an MRI from one hospital looks the same as an MRI from another. This effort is crucial for creating robust AI tools that perform reliably on data from any source and for ensuring consistent diagnostic performance everywhere.
Conclusion
High-quality prostate MRI does not happen by accident. It is the result of a concerted effort to minimize and correct for a wide range of potential artifacts. From careful patient preparation and protocol optimization to the application of advanced post-processing and AI-powered tools, every step is critical. Ultimately, clean, artifact-free images form the essential foundation for reliable lesion detection, accurate PI-RADS scoring, and robust AI-assisted classification. By prioritizing image quality, we empower clinicians with the clarity they need to make confident, life-changing diagnoses.
Pioneering Cancer Detection with AI and MRI (and CT)
At Bot Image™ AI, we’re on a mission to revolutionize medical imaging through cutting-edge artificial intelligence technology.
Contact Us


