Blog
Diffusion-Weighted Imaging (DWI) and Apparent Diffusion Coefficient (ADC) in Prostate Cancer Lesion Classification
Magnetic Resonance Imaging (MRI) has transformed our ability to see inside the human body without invasive procedures. For prostate cancer, certain MRI techniques are exceptionally powerful. Two of the most important are Diffusion-Weighted Imaging (DWI) and its quantitative counterpart, the Apparent Diffusion Coefficient (ADC). These sequences provide critical information about tissue structure at a microscopic level, helping radiologists detect and classify suspicious lesions with greater confidence. By measuring how water molecules move within the prostate, DWI and ADC help distinguish between healthy tissue and dense, potentially cancerous growths. This functional insight is a cornerstone of modern prostate MRI and a key reason why it is so effective for accurate lesion classification.
Understanding Diffusion-Weighted Imaging (DWI)
What is DWI and how it works in prostate MRI
Diffusion-Weighted Imaging (DWI) is a specialized MRI sequence that measures the random motion—or diffusion—of water molecules within tissue. In a healthy, loosely packed prostate tissue, water molecules can move around quite freely. However, in areas with high cellular density, such as a cancerous tumor, this movement is restricted. The cells are packed so tightly together that they create barriers, limiting how far water can travel.
DWI is specifically designed to be sensitive to this restriction. The imaging sequence applies magnetic gradients that cause freely moving water molecules to lose their signal, while water molecules with restricted movement retain their signal. As a result, areas of high cellular density appear “bright” on DWI scans. This makes diffusion-weighted imaging prostate cancer a vital tool, as it provides a functional map of cellularity that complements the anatomical information from other prostate lesion MRI sequences. The unique contrast provided by DWI prostate MRI helps radiologists quickly identify suspicious areas that warrant further investigation.
Interpreting DWI images in prostate cancer
When a radiologist reviews a prostate MRI, the DWI sequence is a primary indicator of potential trouble. Cancerous lesions typically appear as focal areas of high signal intensity—or bright spots—on the high b-value DWI images. This brightness signifies restricted water diffusion, a hallmark of densely packed cancer cells.
However, a bright spot on DWI alone isn’t enough for a diagnosis. Other conditions, like inflammation, can also restrict water movement. This is where the ADC map becomes essential. A true cancerous lesion will typically be bright on DWI and correspondingly dark on the ADC map. This “bright on DWI, dark on ADC” pattern is a classic sign of a clinically significant lesion. Radiologists analyze these signal intensity patterns to evaluate the likelihood of malignancy and correlate their findings with what is known about the underlying pathology of prostate tumors.
Apparent Diffusion Coefficient (ADC): Quantifying Tissue Diffusion
What ADC maps represent and how they’re calculated
While DWI provides a qualitative visual of restricted diffusion (the bright spots), the Apparent Diffusion Coefficient (ADC) map gives us a quantitative measurement. An ADC map is not a direct scan but is mathematically calculated from a series of DWI images acquired at different gradient strengths, known as b-values. By comparing how the signal from water molecules fades at these different b-values, the software can calculate a specific diffusion value for each pixel in the image.
These values are then compiled into an ADC map, where the brightness of each pixel represents how freely water can move. Low ADC values (appearing dark on the map) indicate highly restricted diffusion, whereas high ADC values (appearing bright) signify unrestricted diffusion. This makes the apparent diffusion coefficient MRI a powerful tool for objectively measuring tissue characteristics, turning a visual observation into hard data. When evaluating ADC prostate cancer findings, these quantitative values provide a more objective measure of a lesion’s cellularity.
ADC thresholds and lesion grading
The quantitative nature of ADC maps allows for a more standardized assessment of prostate lesions. Lower prostate cancer ADC values are strongly correlated with higher tumor cellularity and, consequently, more aggressive cancer. Research has established that ADC values can help predict a lesion’s Gleason score, a system used by pathologists to grade the aggressiveness of prostate cancer.
For example, a very low ADC value (e.g., below 750 µm²/s) is highly suspicious for a clinically significant, high-grade cancer. In contrast, higher ADC values are more indicative of benign tissue or low-grade, less aggressive tumors. While there is no universal, definitive threshold due to variations in scanners and techniques, these quantitative ranges provide radiologists with crucial data for grading lesions. This information helps guide decisions about whether a biopsy is needed and what the most appropriate treatment path might be.
Clinical Applications of DWI and ADC in Lesion Classification
Detecting clinically significant prostate cancer
One of the most important roles of DWI and ADC is helping radiologists identify clinically significant prostate cancer—the type that is aggressive enough to require treatment. Within the Prostate Imaging Reporting and Data System (PI-RADS), DWI is a dominant sequence for assessing lesions in the peripheral zone of the prostate.
Lesions that show markedly restricted diffusion (very bright on high b-value DWI and very dark on ADC) are often assigned a PI-RADS 4 or 5 score. These scores indicate a high or very high likelihood that clinically significant cancer is present. By flagging these aggressive lesions, DWI and ADC help ensure that patients who need immediate attention receive it, while potentially sparing men with benign conditions or indolent cancers from unnecessary biopsies.
Differentiating benign vs malignant findings
While DWI and ADC are excellent at detecting cancer, they are not perfect. Certain benign conditions can mimic the appearance of cancer on diffusion imaging. For example, prostatitis (inflammation of the prostate) or benign prostatic hyperplasia (BPH) nodules can sometimes show restricted diffusion, leading to potential false positives.
This is where a radiologist’s expertise, combined with information from other MRI sequences like T2-weighted imaging, becomes critical. An experienced reader can often identify subtle signs that distinguish inflammation or a benign nodule from a true malignancy. Despite these challenges, the information from DWI and ADC provides an invaluable layer of functional data that significantly improves diagnostic accuracy compared to anatomical imaging alone.
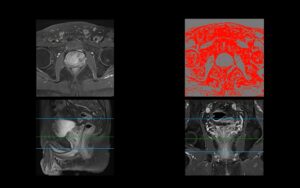
Integrating DWI/ADC findings into AI-assisted classification
The quantitative and standardized nature of DWI and ADC data makes it ideal for analysis by artificial intelligence. AI models, particularly those based on deep learning and radiomics, can process the vast amount of pixel-level information contained in diffusion maps to identify patterns that may be too subtle for the human eye to detect. These models are trained on thousands of MRI scans with known outcomes, learning to associate specific diffusion features with cancer presence, location, and aggressiveness. By leveraging this data, AI can provide a powerful second look, helping to improve the accuracy and consistency of lesion classification.
Technical Considerations and Pitfalls
Optimizing b-values for prostate MRI
The quality of DWI and ADC maps depends heavily on the technical parameters used during the scan, particularly the “b-values.” A b-value reflects
the strength and duration of the diffusion-sensitizing gradients. Prostate MRI protocols typically use a range of b-values, often from 50 s/mm² up to 2000 s/mm².
Low b-values provide good signal-to-noise ratio (SNR) but are less sensitive to diffusion, while very high b-values are highly sensitive to restricted diffusion but suffer from lower SNR. Choosing the right b-values involves a tradeoff between sensitivity and image quality. Most modern protocols include at least one high b-value (e.g., ≥1400 s/mm²) to maximize the contrast between cancerous and benign tissue.
Common artifacts and how to reduce them
DWI is susceptible to several types of image artifacts that can degrade quality and complicate interpretation. Rectal gas, for instance, can cause significant distortion in the surrounding prostate tissue on the image. Patient motion, even slight movements, can lead to blurry or misaligned images, making ADC calculation unreliable.
Radiology departments use various methods to mitigate these issues. Patients may be asked to follow specific dietary instructions to reduce gas. Technologists work to make patients comfortable to minimize motion, and advanced software can correct for certain types of distortion. Overcoming these challenges is key to acquiring high-quality, diagnostically useful diffusion images.
Reproducibility and harmonization across scanners
A significant challenge in using quantitative ADC values is that they can vary between different MRI scanners. Differences in magnet strength, gradient systems, and software can all affect ADC measurements. This lack of standardization can make it difficult to apply a single ADC threshold across different hospitals or imaging centers.
To address this, researchers are working on harmonization techniques to standardize ADC measurements. This involves using imaging phantoms and advanced post-processing algorithms to calibrate data from different scanners. Achieving better reproducibility is crucial for large-scale clinical trials and for training robust AI models that can perform reliably on data from any institution.
The Role of DWI and ADC in Multiparametric MRI (mpMRI)
Combining DWI with T2 and DCE for improved accuracy
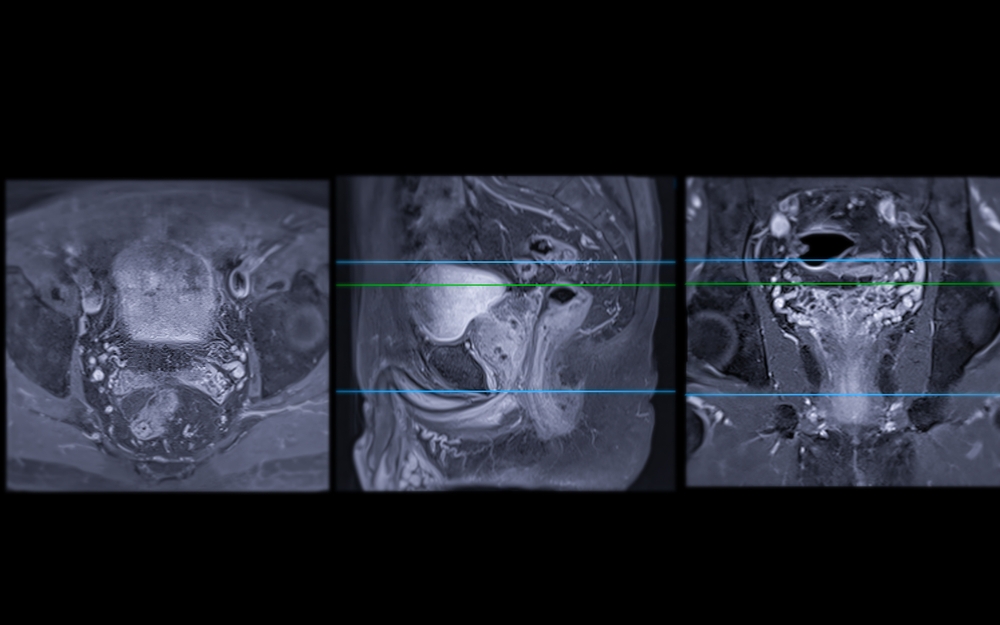
DWI and ADC are almost never used in isolation. They are part of a multiparametric MRI (mpMRI) exam, which combines them with T2-weighted (T2W) and, in some cases, Dynamic Contrast-Enhanced (DCE) imaging. Each sequence provides a unique piece of the puzzle.
T2W imaging offers detailed anatomical information, showing the structure of the prostate and the lesion’s location. DWI provides functional data on cellular density. DCE, which involves injecting a contrast agent, assesses blood flow and vessel permeability. By combining these three perspectives, radiologists can characterize prostate lesions with much higher accuracy, which is the foundation of the PI-RADS scoring system.
Quantitative imaging and radiomics using DWI/ADC maps
The quantitative data from ADC maps is a rich source for radiomics, an advanced field of medical imaging analysis. Radiomics involves extracting a large number of quantitative features from medical images, such as shape, intensity, and texture. ADC-based texture features, which describe the heterogeneity of diffusion within a lesion, have been shown to enhance the performance of diagnostic models. For example, a tumor with highly variable ADC values may be more heterogeneous and potentially more aggressive. By analyzing these complex features, radiomics aims to build more powerful predictive models for diagnosis, prognosis, and treatment response.
Future Directions
Advanced diffusion models (IVIM, DKI, NODDI)
While DWI and ADC provide a robust model of water diffusion, they are a simplification of a complex biological process. Researchers are now exploring more advanced diffusion models to capture even more microstructural detail. These include:
- Intravoxel Incoherent Motion (IVIM): Separates the effects of pure molecular diffusion from micro-perfusion (blood flow in tiny capillaries).
- Diffusion Kurtosis Imaging (DKI): Measures the non-Gaussian behavior of water diffusion, providing insight into tissue complexity.
- Neurite Orientation Dispersion and Density Imaging (NODDI): A sophisticated model that can estimate the density and arrangement of tissue compartments.
These advanced techniques promise to deliver even more specific biomarkers for characterizing prostate tissue.
Integration with AI-driven classification and radiomics pipelines
The future of prostate MRI lies in the seamless integration of these advanced imaging techniques with powerful AI-driven pipelines. As AI models become more sophisticated, they will be able to process data from IVIM, DKI, and other sequences to create comprehensive, multidimensional profiles of tumors. A major focus of current research is the harmonization of these complex diffusion features, which will enable the training of large, multi-institutional AI models that are robust, generalizable, and highly accurate. This synergy will further enhance diagnostic precision and personalize patient care.
Conclusion
Diffusion-Weighted Imaging (DWI) and the Apparent Diffusion Coefficient (ADC) are indispensable tools in the modern diagnosis of prostate cancer. By providing a window into the cellular density of tissue, they empower clinicians to detect, characterize, and classify suspicious lesions with remarkable accuracy. From serving as a cornerstone of the PI-RADS system to fueling the engine of advanced AI algorithms, diffusion imaging is fundamental to both traditional radiology and the future of computer-assisted diagnostics. Its ability to deliver quantitative, functional data helps distinguish aggressive cancers from benign conditions, guiding more confident and effective clinical decisions.
Bot Image’s ProstatID™ leverages the power of DWI and ADC within a bi-parametric MRI (bpMRI) workflow to deliver fast, accurate, and actionable insights. Learn how our FDA-cleared AI software can help you enhance diagnostic confidence and streamline your prostate cancer care pathway.